At present, the overall success rate in clinical trials of new drugs whose efficacy has been demonstrated in animals is only around 10%, as animal models fail to predict human toxicity in at least 50% of cases.
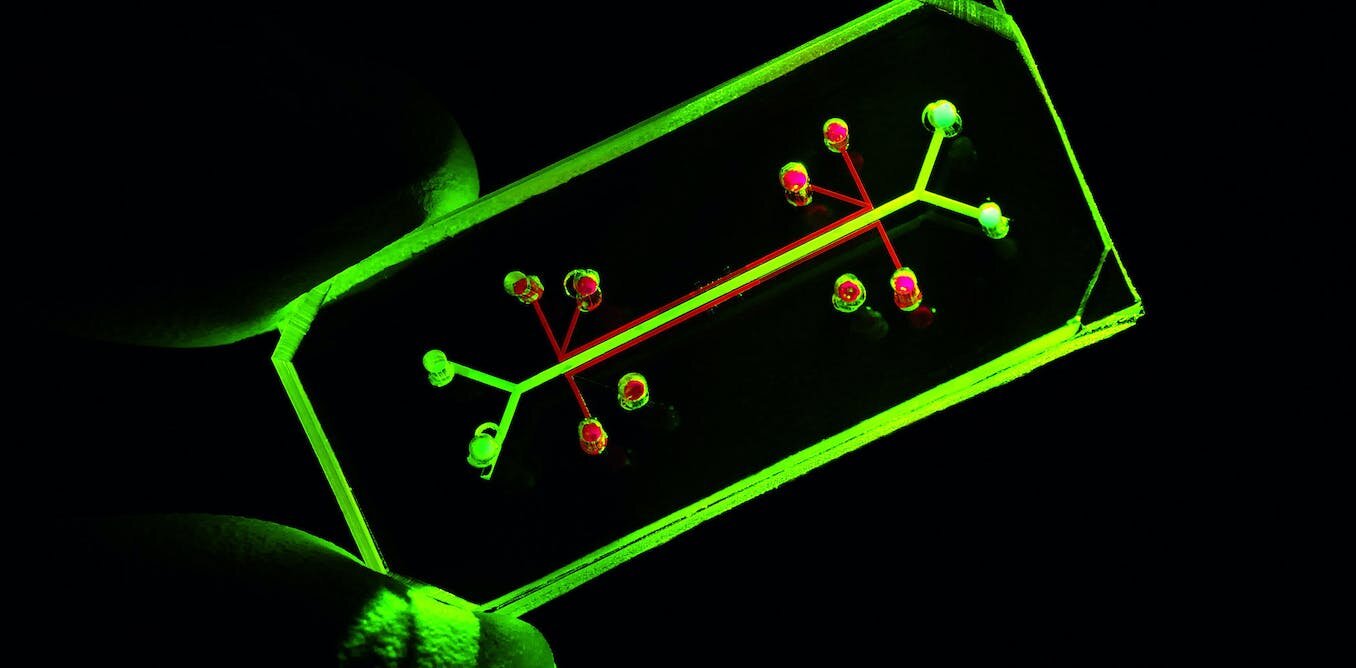
In general, animal models are often inadequate for exploring human disease mechanisms, and raise ethical issues. On the other hand, current in vitro cell cultures poorly mimic in vivo mechanisms and do not easily address patient variability, a key issue for personalized medicine. Organs and organoids on a chip (O&OoC) are emerging as a key innovation, providing human in vitro models that faithfully reproduce in vivo conditions. At the confluence of cell and tissue engineering and microfluidics, O&OCs are miniaturized devices containing living organ substructures in a controlled microenvironment. They can reproduce one or more aspects of the architecture, dynamics and functions of an organ, or even several interconnected organs, with the possibility of controlling different functions in real time.
PEPR MED-OOC is the winner of the third wave of France 2030 calls for projects. It is part of the highly innovative field of personalized medicine via organs and organoids on a chip, and is endowed with funding of 48 million euros over six years.
The main objective of PEPR MED-OOC will be to promote a new generation of OoCs based on patient-derived cells and tissue precursors such as organoids, with the aim of recapitulating the (patho)physiological reality of the patient’s organ, combined with advanced “on-chip” monitoring capabilities.
These O&OoCs will offer:
- researchers, physicians and industry an invaluable alternative to animal models and conventional in vitro models, representative of human phenotypic diversity;
- clinicians, access to standardized “single-organ” or “multi-organ” chips manufactured with patients’ own cells, serving as “clinical twins”, indispensable and dynamic complements to the “digital twins” currently under development.
Note: Priority research programs and equipment (PEPR) aim to build or consolidate French leadership in scientific fields linked to technological, economic, societal, health or environmental transformation, and considered a priority at national or European level.
(Sources: CNRS and CEA websites)
Listen to a replay of the webinar organized by FC3R on December 12, 2024 – Xavier Gidrol (CEA, IRIG) and Anne-Marie Gué (CNRS, LAAS) presented the PEPR framework. Emily Tubbs (CEA, IRIG) presented her advances in pancreas modeling with a view to personalized medicine for type 1 diabetes. Maria-Carla Parrini (Inserm, Institut Curie) detailed tumor-on-a-chip technology and its implications for tomorrow’s personalized medicine.
Towards organs-on-a-chip at the patient’s bedside
Article published on February 20, 2024 on the CNRS website
Interview with Anne-Marie Gué: CNRS Research Director at the Systems Analysis and Architecture Laboratory (CNRS / INSA Toulouse / Toulouse INP / Université Toulouse III Paul-Sabatier).
Q: Could you tell us about the issues surrounding personalized medicine that are behind the PEPR MED-OOC program, which you co-direct with Xavier Gidrol (for CEA) and Jean Rosenbaum (for Inserm)?
Anne-Marie Gué : On the one hand, we observe that the overall success rate in clinical trials of new drugs whose efficacy has been demonstrated in animals is only around 10%. This means that animal models are not sufficiently predictive of toxicity and/or efficacy in humans. On the other hand, current 2D in vitro cellular model systems do not adequately reproduce the physiological or pathological mechanisms that occur in our bodies. Nor can they account for the variability between patients that is one of the central issues in personalized medicine.
In recent years, however, we have seen the emergence of a new type of biological model known as organs and organoids-on-a-chip, depending on how they are constructed. These miniaturized devices contain three-dimensional cell cultures mimicking the functions of living organs or tissues in a controlled microenvironment. These systems can reproduce one or more physiological or pathological aspects. It is also possible to link different organ models together to study their interactions. In this sense, it is a key innovation that could respond to many public health challenges by faithfully reproducing in vivo conditions in human in vitro models.
Q: What are MED-OOC’s objectives?
A-M. G : Until now, organs and organoids on a chip have been produced mainly from cell lines obtained from an original cell or from stem cell cultures. PEPR MED-OOC aims to develop them from patient cells for personalized medicine. These models will then help determine and select the best possible treatment for a given patient. In oncology, for example, it is often necessary to test several therapeutic approaches before finding the right one, as each cancer is unique and each patient has his or her own particularities. In the long term, the challenge will be to pre-test the various treatments not on the patient, but on models derived from his or her tumor, for example, to ensure that the treatment is as effective as possible.
What’s more, these new systems willbenefit reduce the need for animal experimentation, which is also a strong social expectation.
Q: What are PEPR’s main areas of research?
A-M. G : The program covers the entire development chain, from basic research to clinical applications. We have identified three key areas of research. The first is the development of what we call “clinical twins” of patients. We have yet to understand what functional elements need to be implemented as a minimum in organs and organoids-on-a-chip to faithfully represent a patient’s pathology.
The aim of the second axis is to make the devices more complex. For example, by mimicking blood circulation or reconstituting the interactions between several organs, so as to be able to target and validate conventional drugs, immunotherapies and biotherapies. These couplings are essential for the best possible representation of physiological and pathological mechanisms. The final focus will be to instrument these on-chip models with sensors to measure and monitor mimicked functions in real time.
All this research will be applied in priority to three pathologies with a high public health impact: breast cancer, type 2 diabetes and metabolic syndrome (disorders linked, for example, to a diet too rich in sugars and fats, liver failure, obesity, etc.). To this end, we will design and validate organs and organoids on a chip hosting tumors in the case of cancer, pancreatic cells for diabetes, and a liver-adipose tissue coupling in the latter case.
Q: How will PEPR transfer these models from the laboratory to the patient’s bedside?
A-M. G To make organs-on-a-chip from patient cells or explants (tumor samples), we need to bring our developments as close as possible to clinicians, in hospital centers. To this end, we are going to set up a national network of infrastructures specifically dedicated to the implementation of these new models. We will start with four French hospitals: the Institut Curie in Paris, the University Hospitals of Grenoble and Toulouse, and the Paul Brousse Hospital of the AP-HP in Villejuif. These platforms will enable us to finalize the development of our chips with patient cells, and then use them in the hospital environment. We hope that all major hospitals will eventually be able to set up such centers, so that their patients can benefit from these technologies.
Q: What obstacles need to be overcome before this transfer to society can go ahead?
A-M. G The market for personalized medicine is currently developing. Industrialists will have to adopt our technologies in order to manufacture and market the chips. So there’s a whole industrial sector to be created, with applications in medicine and pharmacology targeted by PEPR, but we can also imagine uses in agri-food and cosmetics. Organoids and organs on a chip could, for example, be used for allergy or tolerance testing.
Industrialization will have to take into account all the associated issues of normalization, standardization and certification. In order to work with this in mind, and produce approved products as quickly as possible, we plan to set up a committee within the PEPR MED-OOC to liaise with the health agencies and authorities that issue authorizations for new health technologies, as well as with manufacturers in the field.
This work is also in line with a desire for national sovereignty. It is unthinkable that French hospitals and manufacturers should have to rely on foreign suppliers to provide these strategic healthcare devices, when we have all the necessary capacities in France to be at the cutting edge of these technologies of the future.